In a recent study published within the JAMA Network journal, researchers assessed the association of coronavirus disease 2019 (COVID-19) and influenza with thrombotic events amongst patients.
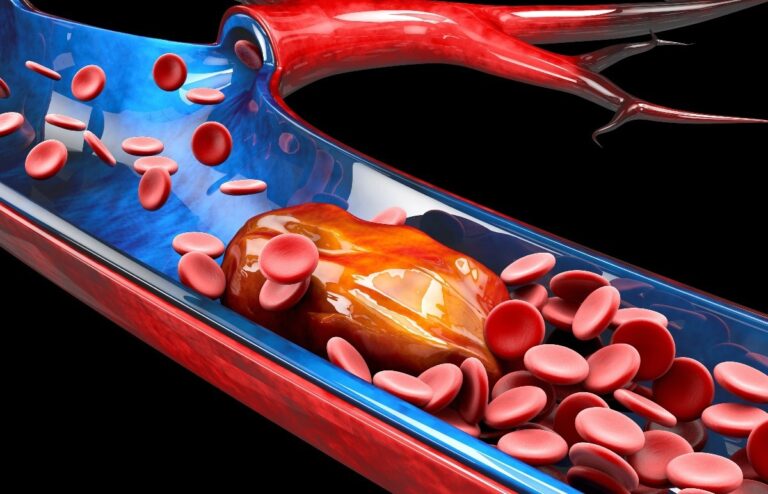
Study: Association of COVID-19 vs Influenza With Risk of Arterial and Venous Thrombotic Events Amongst Hospitalized Patients. Image Credit: Victor Josan/Shutterstock
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is deemed an acute respiratory illness. Nonetheless, studies have reported that COVID-19 could induce a hypercoagulable state resulting in venous and arterial thromboembolism. Almost 30% of COVID-19-hospitalized patients experience thromboembolism. Yet, the incidence, risk aspects, and consequences related to COVID-19-induced thromboembolism still require extensive research.
In regards to the study
In the current study, researchers estimated the 90-day risk of venous and arterial thromboembolism in patients hospitalized as a result of COVID-19 in comparison with patients hospitalized as a result of influenza.
The team performed a retrospective cohort study with data collected from the US Food and Drug Administration (FDA) Sentinel System. Participants included within the COVID-19 cohort were those (1) who had a history of initial COVID-19 International Classification of Diseases-10 (ICD-10) diagnosis code or a positive nucleic acid test result for COVID-19 recorded between 1 April 2020 and 31 May 2021, (2) aged 18 years and above on the time diagnosis, and (3) having continuous pharmacy and medical coverage during diagnosis of three hundred and sixty five days or longer.
Participants eligible for the influenza cohort included (1) patients with an initial ICD-10 diagnoses code for influenza or a positive nucleic acid test result for influenza recorded between 1 October 2019 and 30 April 2019, (2) patients aged 18 years and above on the time of diagnosis, and (3) patients having continuous pharmacy and medical coverage during diagnosis of three hundred and sixty five days or longer. The study included patients diagnosed within the influenza season between 2018 and 2019 to be sure that the influenza patients weren’t co-infected with COVID-19.
The first outcomes of the study included (1) inpatient arterial thromboembolism, which was defined as a contributory or principal hospital discharge diagnosis of ischemic stroke or acute myocardial infarction, and (2) inpatient venous thromboembolism which was defined as a contributory or principal hospital discharge diagnosis of pulmonary embolism or acute deep vein thrombosis. The secondary consequence included an expanded arterial thromboembolism endpoint and an expanded venous thromboembolism end-point. The first and secondary outcomes for thrombotic events were recorded for influenza patients through 29 July 2019 and COVID-19 patients through 29 August 2021.
Results
The study results showed that 41,443 patients were COVID-19-hospitalized before the SARS-CoV-2 vaccines were made available, 44,194 patients were COVID-19-hospitalized when the vaccines were available, and 8269 patients were influenza-hospitalized. In comparison with influenza cohorts, the COVID-19 cohorts included patients who were comparatively older and had a lower variety of White and feminine patients with the next proportion of patients having comorbidities. Compared with COVID-19 patients, influenza patients had the next prevalence of asthma, heart failure, chronic obstructive pulmonary disease (COPD), and allotted corticosteroids.
The 90-day absolute risk of experiencing arterial thromboembolism was 14.4%, 15.8%, and 16.3% amongst patients hospitalized as a result of influenza, and COVID-19 before and after the supply of vaccines, respectively. In each patient group, the 90-day risk of arterial thromboembolism was remarkably higher in patients who were male, older, hospitalized within the intensive care unit (ICU), needed mechanical ventilation, or had a previous record of heart problems. Notably, amongst COVID-19 patients across all study groups, the risks related to arterial thromboembolism were comparable.
Moreover, the chance of arterial thromboembolism was not remarkably higher amongst COVID-19 patients before vaccine availability than after the vaccines were made available. Moreover, the association of arterial thrombosis was comparable with a hospital or emergency department discharge diagnosis of ischemic stroke, acute myocardial infarction, transient ischemic attack, peripheral artery disease, or angina amongst COVID-19 patients before and through vaccine availability. Comparing the incidence of arterial thrombotic events amongst influenza patients, 30-day all-cause mortality was remarkably higher amongst COVID-19 patients before and through vaccine availability.
The team also noted that the 90-day absolute risk of venous thromboembolism amongst patients hospitalized with influenza, and COVID-19 before and through vaccine availability was 5.3%, 4.1%, and 10.9%, respectively. Moreover, in each patient group, the 90-day risk of venous thromboembolism was elevated amongst patients admitted to the ICU, who needed mechanical ventilation, or had a previous venous thrombotic event.
When patients who didn’t have a previous record of venous thromboembolism were in comparison with those with influenza, the chance of experiencing venous thromboembolism was higher for COVID-19 patients before and through vaccine availability. Furthermore, amongst patients having a previous record of venous thromboembolism and patients with influenza, the chance of reporting subsequent venous thromboembolism was not considerably higher amongst COVID-19 patients before vaccination ability in comparison with that in vaccine availability.
Overall, the study findings highlighted a major correlation between hospitalized COVID-19 patients and hospitalized influenza patients with the next risk of experiencing venous thromboembolism inside 90 days.